
This is the second in a two-part series on the use of compound drugs in workers' compensation.
The Hartford is one of the largest players in the workers’ compensation space and as its medical director, Dr. Robert Bonner has a privileged view of trends emanating from the market. One of the most concerning is the increase in prescription of potentially dangerous compound drugs to treat injured workers.
“Over the past several years, we were seeing an increase in the number and variety of compounds used in the workers’ compensation space—especially topical,” Dr. Bonner told Insurance Business. “The question that was raised was just how effective those prescriptions were. Is it making a difference for patients, and is The Hartford’s experience similar to the rest of the industry?”
Bonner voiced his concerns to Joseph Paduda of the trade group CompPharma. The result was CompPharma’s recent release of a research paper detailing the use of compounds and their effect on worker safety and comp costs.
The paper concluded that while no clinical evidence has been provided to support the increased use of compound medication, physicians continue to prescribe the drugs to injured workers. According to additional research from the California Workers Compensation Institute, the drugs are roughly three times as expensive as commercially available prescriptions and may even keep employees out of the workplace longer, racking up medical and indemnity costs.
Bonner, who served as the medical advisor on the CompPharma research paper, said the results “raise concerns when physicians use [compounds] as their first line of defense.” And while compounding is a problem in most states, physicians in some areas are more prone to prescribe the drugs than in others.
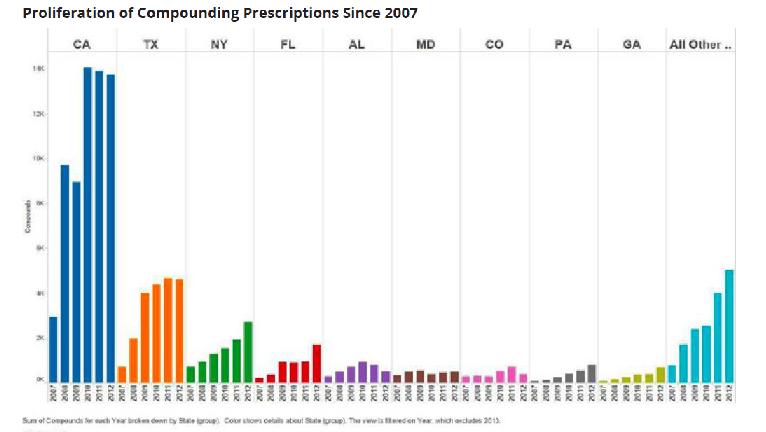
According to CompPharma research, California, Texas, New York, Florida, Alabama, Maryland, Colorado, Pennsylvania and Georgia lead the pack when it comes to the increased issuance of compounded prescriptions since 2007.
Paduda earlier told Insurance Business one of the driving forces behind the proliferation of compounds is self-interested physicians who hope to profit from the higher prices. Bonner was not so quick to condemn, noting that physicians likely "think they’re acting in the best way to provide pain relief," and follow the prescribed methods of the area in which they practice.
“I think most of the time, physicians don’t go into the office and say ‘How can I rip off the system?” Bonner said. “They say, ‘How can I help the patient?’ It just so happens that the science behind the use of compounds in medication shows they’re pretty much ineffective.”
Bonner said any regulation regarding the use of compounds would likely have to come from the states. However, some carriers—like The Hartford—have pharmacy review programs that challenge the use of questionable prescriptions and require doctors to provide a scientific explanation to support their use in each individual case.
Like Paduda, Bonner also places great importance on the role of the insurance agent in protecting injured workers from the potential harms of compound drugs.
“With regard to agents placing business with various workers’ compensation carriers, they have an opportunity to review the individual carrier and see what they are doing with regard to this issue,” Bonner said. “An ideal carrier would have identified it as a concern and put steps in place to help manage it.”
Image Source: CompPharma
You may also enjoy: "'Self-interested providers' drive up WC costs with compound drugs"
"Insurer takes over as workers' comp leader"
"Tina Fey isn't laughing after workers' comp suit"
